Abstract
Background
Interim 18F-fluorodeoxyglucose positron emission tomography-computed tomography (PET-CT) scan may predict outcomes in patients with diffuse large B-cell lymphoma (DLBCL). However, overall accuracy in predicting treatment outcomes on adopting 5-point Deauville score (DS) was considerably low in DLBCL because of mainly low positive predictive value of interim PET-CT scans. This suggested that additional tool might be needed to more accurately predict treatment outcomes. International prognostic index (IPI) was greatly associated with outcomes for DLBCL and considered to reflect biologic aggressiveness of DLBCL. Thus, we hypothesized that combined assessments using DS on interim PET-CT scan and baseline IPI might improve the prediction of treatment outcomes in DLBCL patients. In this study, we aimed to establish the risk predicting model integrating DS on interim PET-CT as an estimate of early metabolic response and baseline IPI as a predictor of biologic aggressiveness in patients with newly diagnosed DLBCL.
Methods
In this retrospective cohort study, we consecutively enrolled patients with newly diagnosed DLBCL. Patients were eligible if they were histologically confirmed with DLBCL from Jan 2007 to June 2016, received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone), and had PET-CT scan data at baseline and at interim after 3 cycles of R-CHOP. Primary CNS or transformed DLBCLs were excluded. Interim PET-CT was assessed using 5-point DS and four point or higher was regarded as positive. All PET-CT scans were assessed by 2 experienced nuclear medicine physicians, who were masked to treatment outcomes of the patients. Discrepant interpretations between 2 nuclear medicine physicians were resolved by consensus through mutual discussion.
Results
A total of 316 patients were screened for eligibility. Ninety-six patients were excluded from the analysis due to following reasons: unavailable baseline (n=9) or interim PET-CT scans (n=48), early death before interim PET-CT (n=16), Primary CNS or transformed DLBCLs (n=15), and insufficient medical records (n=8). Thus, 220 patients were analyzed. Median age was 64 years (range, 19-87) and 132 (60%) were male. Based on the IPI risk, patients were classified as the low or low-intermediate (LI; N=126, 57%), and high-intermediate (HI) or high (N=94, 43%) groups. Interim DS was determined as 1 (n=67, 30.5%), 2 (n=65, 29.5%), 3 (n=39, 17.7%), 4 (n=36, 16.4%), and 5 (n=13, 5.9%).
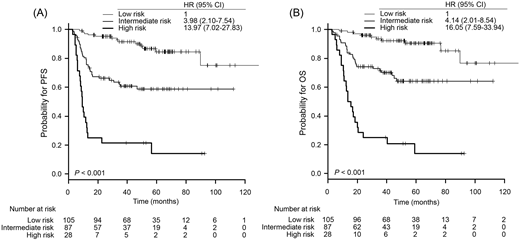
With a median follow-up of 56.6 months (IQR 36.0-71.8), 5-year progression-free survival (PFS) rate was 65.2% (95% CI, 58.1-72.3) and overall survival (OS) rate was 69.9% (95% CI, 63.2-76.6). Interim DS (1-3 vs 4-5) and the IPI (low-LI vs HI-high) were independently associated with PFS (for interim DS of 4-5, hazard ratio [HR], 2.96 [95% CI, 1.83-4.78], P < 0.001; for HI-high IPI, HR, 4.84 [2.84-8.24], P < 0.001) and OS (for interim DS of 4-5, HR, 2.98 [1.79-4.98], P < 0.001; for HI-high IPI, HR, 5.75 [3.14-10.51], P < 0.001) in the multivariate analysis. We stratified patients into 3 groups based on the risk of progression: Low (low-LI IPI and interim DS 1-3), Intermediate (low-LI IPI with interim DS 4-5, or HI-high IPI with interim DS 1-3), and High (HI-high IPI and interim DS 4-5) risk groups. The risk stratification model showed a significant association with PFS (for low risk vs intermediate risk, HR 3.98 [95% CI, 2.10-7.54], P<0.001; for low risk vs high risk, HR 13.97 [7.02-27.83], P<0.001; Fig 1A) and OS (for low risk vs intermediate risk, HR 4.14 [2.01-8.54], P<0.001; for low risk vs high risk, HR 16.05 [7.59-33.94], P<0.001; Fig 1B).
Conclusion
Combining interim DS with baseline IPI can improve risk stratification in patients with newly diagnosed DLBCL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.